(Real Clear Investigations) Abortion rights advocates hoping to make it easier to end later-term pregnancies have outsourced a potentially dangerous drug trial to an impoverished African country.
The clinical trial in Burkina Faso is testing the efficacy of second-trimester abortions using a two-drug combination that includes RU-486, which is currently used in a growing number of first-trimester abortions. Excessive bleeding is a common side effect of the drug, leading some to question the ethics of conducting the trial in a country with limited medical facilities and blood supplies.
In an interview in Ouagadougou, Burkina Faso’s capital, the study’s director, Dr. Blandine Thieba, confirmed that blood supplies are an ongoing concern.
“Right now there are big problems of need in blood bags,” she told RealClearInvestigations, “but fortunately, thanks to God we did not have a case that required a transfusion.”
[Click here to subscribe to Pregnancy Help News!]
The outsourcing of the study, which began 2½ years ago, appears to reflect the reluctance of American women to participate in such trials. In a recent illustration, researchers writing in a 2013 bulletin from the American College of Obstetricians and Gynecologists acknowledged that they had failed to recruit enough women for a North Carolina study of mid-term, drug-induced abortions. Reason: Potential participants “strongly preferred” surgical abortion, which is normally performed with anesthesia, while drug-induced abortions typically are not, even though they can be physically and emotionally distressing. The researchers recommended outsourcing such trials to Europe or Asia.
Tweet This: "The outsourcing of the study, which began 2½ years ago, appears to reflect reluctance of American women to participate in such trials"
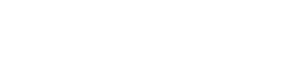
The Burkina Faso trial is sponsored by Gynuity Health Projects, a New York-based group aligned with Planned Parenthood, the largest abortion provider in the United States.
Gynuity’s literature boasts that it is a “a small team willing to take risks on the frontiers of reproductive and maternal health.” One of those efforts seeks to “increase availability and market sustainability of mifepristone” – another name for RU-486 – with a United States-approved protocol that might not even require a visit to a doctor or clinic.
In separate, federally approved research being conducted in 10 American states from Hawaii to New York, Gynuity is testing whether it is safe for doctors to prescribe abortion drugs through telephone or Internet consultations. The Food and Drug Administration now requires abortion drugs to be administered under the supervision of a doctor who can perform surgery or has access to a physician who can in case of emergency.
Tweet This: The FDA requires abortion drugs to be administered under the supervision of a doctor who can perform surgery/with access to one who can ..
It is not clear whether abortion rights advocates envision second-trimester abortions using such “telemedicine.” But the research in Burkina Faso and the U.S. is happening as the advocates redouble efforts against what they see as threats to abortion access posed by a conservative-leaning Supreme Court and restrictive new state abortion laws.
More lenient abortion procedures might gain wider acceptance if they are certified as safe and offer greater privacy, and assuming liberal states set a trend by adopting them. While several states have imposed new abortion restrictions, others such as New York, Illinois, Vermont, and Rhode Island have adopted new abortion protections.
“The Supreme Court is looming large over these state debates,” Elizabeth Nash, a policy analyst at the Guttmacher Institute, an abortion rights advocacy group, told the Pew Charitable Trust’s Stateline website recently. “The last time that people thought Roe was in this kind of jeopardy was the early 1990s. That’s the only other time we saw Democratic-led states adopt protections for abortion.” She was referring to the landmark 1973 Supreme Court decision Roe v. Wade, which protects a pregnant woman's right to have an abortion without excessive government restriction.
Current FDA guidelines approve mifepristone abortions only through the first 70 days of pregnancy, or roughly the first trimester of a nine-month pregnancy. But state laws vary, and American doctors are known to perform later abortions “off-label.” Drug-induced second-trimester abortions are performed in European countries, although usually with restrictions.
These drugs should not be confused with the contraceptive morning-after pill. The Mayo Clinic’s website explains that morning-after pills – the over-the-counter drug levonorgestrel or the prescription drug ulipristal acetate – “do not end a pregnancy that has implanted. They work primarily by delaying or preventing ovulation.”
According to the Guttmacher Institute, more than 850,000 abortions are performed in the United States each year with about 90 percent occurring the first trimester. Surgical abortions comprise 61% of the total. Drug-induced abortions, which normally occur during the first 10 weeks of pregnancy, accounted for 39% of the total in 2017 – up from just 5% in 2001 and 29% in 2014.
Gynuity did not respond to RealClearInvestigations’ inquiries about the Burkina Faso trial, although Dr. Thieba was interviewed in the country in late November by a freelance journalist hired by RCI. Abortion rights advocates such as Planned Parenthood, NARAL, and the Guttmacher Institute all declined to talk with RealClearInvestigations about abortion research and related ethical considerations. Officials at the State Department and federal health agencies also declined.

Tweet This: "Planned Parenthood, NARAL and the Guttmacher Institute all declined to talk [] about abortion research and related ethical considerations"
Public documents shed some light on the study, however. A description based on information provided by Gynuity was posted in August 2017 on the federally maintained research database ClinicalTrials.gov. It said an “estimated” 100 women with “an ongoing pregnancy of 13-22 weeks gestation” – that is, in their second trimester – were to be recruited to participate in the study.
The trial, to begin in May 2017 and end Dec. 31, 2019, would be conducted in four cities in Burkina Faso: Ouagadougou, Bobo-Dioulasso, Boromo, and Ouahigouya. Patients in the study had to “be willing to undergo surgical completion if necessary” – surgical abortion – in the event of complications, and to provide consent.
It is not clear how the women were recruited for the study, and details of Gynuity’s role in supporting this research could not be ascertained, including how much funding it provided, and whether doctors affiliated with Gynuity traveled to Burkina Faso to supervise or work on the study.
The U.S. government website states that the goal of the Burkina Faso trial is “to examine the effectiveness and feasibility of a mifepristone-misoprostol medical abortion regimen” in the second trimester.
Mifestrone blocks progesterone, a hormone vital to fetal development, delivered from the mother through the placenta and umbilical cord, and kills the fetus. Another drug, misoprostol, administered later, causes the uterus, where the fetus was conceived, to shrink, expelling the detached embryo through the vagina.
At 19 weeks – or mid-second trimester -- a typical fetus is about 6 inches long and weighs about 8 ounces. Medical News Today reports that “the fetus may be developing hair on its head. The kidneys of the fetus will now be making urine. A female fetus now has six million eggs in her ovaries.”

Abortions in these circumstances are more likely to lead to potentially life-threatening complications for the mother, including cervical laceration, infection, and uterine rupture.
A 2009 study on women in Finland published in Obstetrics & Gynecology found that one out of every five given abortion drugs in the first trimester experienced some kind of complication. The most common adverse effect was potentially life-threatening hemorrhaging, which represented 16% of the total complications.
Doctors with experience in the region doubt that such research is ever advisable in places such as Burkina Faso. The landlocked, recurrently unstable former French West African colony has one physician for roughly every 16,000 people, and one hospital bed for every 2,500 people, in a nation of over 19 million, according to the CIA World Factbook. There are currently about 100 gynecologists in the Society of Gynecologists and Obstetricians of Burkina Faso, RCI’s reporting established. The CIA also reports that the country has one of the highest infant-mortality rates (72 deaths per 1,000 live births) and lowest life expectancy rates (56 years) in the world.
The numbers may help explain why the Guttmacher Institute found that about two-thirds of the 23,000 women treated for abortion-related complications there in 2008 “suffered serious complications but did not receive the care they needed.”
A major problem is chronic shortages of transfusion blood. Dr. Christina M. Francis, an OB-GYN who’s done extensive work in Kenya, Burma, Afghanistan, and other developing countries, said: “In general, throughout Africa, regardless of whether you're in this big city or a small village, blood products tend to be difficult to come by. There are national shortages very frequently.”
Dr. Francis, who is affiliated with the Charlotte Lozier Institute, a scientific research organization that does work from a pro-life/anti-abortion perspective, continued: “And so, even if you've got a woman in, say, the biggest hospital in the capital of Burkina Faso, that doesn't mean that she's going to have access to blood products just because she's in that hospital.”
The study director in Burkina Faso, Dr. Thieba, confirmed that “the availability of blood is most often a real problem.” But, she said, “as soon as the woman realizes that she is bleeding a lot, she comes and we end the abortion with the aspiration [vacuum suction]; we do not continue, because if we let the medicine act it will take time; the bleeding will be prolonged.”
Dr. Thieba said there is a “tracking protocol” for the women in the study that ensures regular follow-ups until the abortion is completed, but the lack of hospital beds and medical facilities means that women cannot be monitored after the mifepristone and misoprostol are administered. “When we prescribe, we explain the signs of danger to women and, as soon as these signs appear, they come,” she said. "Most often, they have provider contact."
The Guttmacher Institute estimates that between 2% and 4% of pregnancies in Burkina Faso end in abortion. Dr. Thieba said drug-induced abortions may be useful because a lack of anesthesia and anesthesiologists are impediments to safe surgical abortions.
An abortion-related drug trial in a developing country raises other concerns because of the West’s past influence over population-control efforts that have adversely affected women.
In 1972, the International Planned Parenthood Federation sponsored an experiment to terminate the pregnancies of hundreds of Bangladeshi women who had been raped by Pakistani soldiers. A number of the pregnancies were ended using an unproven device known as a “super coil,” developed by a psychologist with no formal medical training. The device was later described in a court case as "basically plastic razors that were formed into a ball” and would spring open inside a woman’s uterus. It resulted in a high rate of complications.
While there are few specifics on what happened to the women in Bangladesh, the super coil was used on one occasion in America later that year; 13 out of 15 women had to be hospitalized with serious complications, and one of them had to have a hysterectomy.
No charges were brought at the time against the Philadelphia doctor who used the device, Dr. Kermit Gosnell. He would become infamous decades later when he was convicted of first-degree murder and a host of other crimes in 2013 related to his operation of an abortion clinic in Philadelphia.
In India in 1975, Prime Minister Indira Gandhi declared overpopulation a national emergency and created a large-scale, mandatory sterilization program. The Ford Foundation backed the effort, providing the infrastructure that made the sterilization programs possible.
The drug being tested in Burkina Faso is connected to abortion research's international past. Mifepristone was developed in France, and in 1994 a nonprofit American group called the Population Council “was given the rights to sell RU-486 by French drug maker Roussel Uclaf SA, which was put off by the controversy surrounding the drug in the United States,” the Washington Post reported in 2000, the year the drug was approved for use in the United States.
The Population Council was founded by John D. Rockefeller III in the 1950s with a mission rooted in population control and eugenics. In Donald T. Critchlow’s book “Intended Consequences: Birth Control, Abortion, and the Federal Government in Modern America,” the organization’s mission and motives are made clear:

An initial draft charter of the council submitted by Rockefeller called for the promotion of research so that "within every social and economic grouping, parents who are above the average in intelligence, quality of personality and affection, will tend to have larger than average families."
This paragraph would be dropped when Thomas Parran, a Catholic and former surgeon general, told Rockefeller, "Frankly, the implications of this, while I know are intended to have a eugenic implication, could readily be misunderstood as a Nazi master race philosophy."
Gynuity also illustrates ties between population control advocates and abortion rights advocates. Before she became president of Gynuity in 2003, Dr. Beverly Winikoff had spent 25 years working at the Population Council.
The clinical trial in Burkina Faso also resonates with the history of abortion drugs in the United States. Aside from the involvement of the Population Council in producing RU-486, the Buffet Foundation provided millions of dollars to perform clinical trials on mifepristone for U.S. approval.
Approving the drug in 2000 was a major priority for the soon-departing Clinton administration, which took extraordinary steps to fast-track the process. Mifepristone approval was expedited through an FDA regulation known as “Subpart H,” which was meant only for “Accelerated Approval of New Drugs for Serious or Life-Threatening Illnesses” where existing treatments are either insufficient or nonexistent.
The FDA approval process for mifepristone was unusual in other ways. “FDA Commissioner Jane E. Henney said the agency broke with precedent by not publishing the names of the experts who reviewed RU-486 for the agency,” the Washington Post reported. “In another first, it did not publish the name or location of the company that will manufacture the drug.”

Eventually, it was reported that the drug was manufactured by a pharmaceutical company formed in the Cayman Islands in 1995 named Danco, which continues make the drug. After the formation of Danco, the David and Lucile Packard Foundation – of Hewlett-Packard fame – lent it $10 million to help with marketing and FDA approval.
To this day, little is known about Danco Laboratories, beyond the names of a few of its top officers and that it is based in New York City. Abortion advocates insist that such secrecy is necessary for the safety of those who work at the company.
The Trump administration hasn’t publicly expressed concern, though it has touted its "Protecting Life in Global Health Assistance" policy, aimed at ending U.S. government funding of international abortion efforts.
Despite RCI’s multiple requests for comment from the State Department, National Institutes of Health, the U.S. Agency for International Development, and the Department of Health and Human Services’ Office of Global Affairs, no government official would speak on the record about chemical abortion research and the issues involved in international clinical trials. The only response was a statement from an HHS spokesperson: “The U.S. government has oversight of international clinical trials if they are federally funded, or if the trial is privately funded and is being conducted to support an application to FDA for a new drug or device.”
Tweet This: No (US) government official would speak on the record about chemical abortion research and issues involved in international clinical trials
If Gynuity’s studies regarding chemical abortion and telemedicine are successful, they might make it widely possible for women seeking abortions to perform them themselves, leaving legal restrictions on abortion exceedingly difficult to enforce. Pro-life groups raise alarms about the safety of such a situation.
“The end game, the ultimate goal for the pro-abortion side, is to have a powerful abortion drug available over the counter,” said Dr. Donna Harrison, an OB-GYN and executive director of the American Association of Pro-Life Obstetricians and Gynecologists.
Tweet This: “The end game, the ultimate goal for the pro-abortion side, is to have a powerful abortion drug available over the counter”
“If they can generate some studies that say, 'Oh, this is safe' -- whatever 'safe' means in the second trimester -- then they can argue, 'Oh, it doesn't matter if women don't know how far along they are.' It's quote 'safe,' ”
Editor's Note: This report was first published by Real Clear Investigations. Heartbeat International, which manages Pregnancy Help News, also manages the Abortion Pill Rescue Network.